Rehabilitation
Overview
Rehabilitation is defined as “a set of interventions designed to optimize functioning and reduce disability in individuals with health conditions in interaction with their environment”.
Put simply, rehabilitation helps a child, adult or older person to be as independent as possible in everyday activities and enables participation in education, work, recreation and meaningful life roles such as taking care of family. It does so by working with the person and their family to address underlying health conditions and their symptoms, modifying their environment to better suit their needs, using assistive products, educating to strengthen self-management, and adapting tasks so that they can be performed more safely and independently. Together, these strategies can help an individual; overcome difficulties with thinking, seeing, hearing, communicating, eating or moving around.
Anybody may need rehabilitation at some point in their lives, following an injury, surgery, disease or illness, or because their functioning has declined with age.
Some examples of rehabilitation include:
:max_bytes(150000):strip_icc()/rehabilitation-therapies-for-multiple-sclerosis-4072854-e72137c8397a4d909ce759135c9fa3a8.png)
- speech and language training to improve a person’s communication after a brain injury;
- physical exercise training to improve muscle strength, voluntary movements and balance in persons with stroke or Parkinson disease;
- modifying an older person’s home environment to improve their safety and independence at home and to reduce their risk of falls;
- educating a person with heart disease on how to exercise safely;
- preparing a person with an amputation to be able to use a prosthetic and making, fitting and refitting the prosthesis;
- positioning and splinting techniques to assist with skin healing, reduce swelling, and to regain movement after burn surgery;
- prescribing medicine to reduce spasticity for a child with cerebral palsy;
- psychological therapies for a person with emotional distress following a spinal cord injury;
- social skills training for persons with schizophrenia, autism spectrum disorders or disorders of intellectual disability.
- training a person with vision loss in the use of a white cane; and
- working with a patient in intensive care to improve their breathing, prevent complications and speed their recovery after critical illness
Rehabilitation is highly person-centred, meaning that the interventions selected for each individual are targeted to their goals and preferences. Rehabilitation can be provided in many different places, such as inpatient or outpatient hospital settings, outpatient physio- or occupational therapy practices, and community settings such as an individual’s home, a school or a workplace.
The rehabilitation workforce is made up of different health workers, including but not limited to physiotherapists, occupational therapists, speech and language therapists and audiologists, orthotists and prosthetists, clinical psychologists, physical medicine and rehabilitation doctors, and rehabilitation nurses. Many other health workers, such as general practitioners, surgeons, and community health workers may also play an important role in a person’s rehabilitation.
The Benefits of Rehabilitation
Rehabilitation can reduce the impact of a broad range of health conditions, including diseases (acute or chronic), illnesses or injuries. It complements other health interventions, such as medical and surgical interventions, helping to facilitate recovery and achieve the best outcome possible. In addition, rehabilitation can help to prevent, reduce or manage complications associated with many health conditions, such as in the context of spinal cord injury, stroke, or fractures.
Rehabilitation helps to minimize or slow down the disabling effects of chronic health conditions, such as cardiovascular disease, cancer and diabetes by equipping people with self-management strategies and the assistive products they require, or by addressing pain or other complications. As such, it contributes to healthy ageing.
Rehabilitation is an investment, with cost benefits for both the individuals and society. It can help to avoid costly hospitalization, reduce hospital length of stay, and prevent re-admissions. As rehabilitation also enables individuals to engage in or return to work and employment, or to remain independent at home, it minimizes the need for financial or caregiver support.
Rehabilitation is an important part of universal health coverage and is a key strategy for achieving Sustainable Development Goal 3 – “Ensure healthy lives and promote well-being for all at all ages”.
Misconceptions About Rehabilitation
Rehabilitation is not only for people with disabilities or long-term or physical impairments. Rather, rehabilitation is an essential health service for anyone with an acute or chronic health condition, impairment or injury that limits functioning, and as such should be available for anyone who needs it.
Rehabilitation is not a luxury health service that is available only for those who can afford it. Nor is it an optional service to try only when other interventions to prevent or cure a health condition fail.
For the full extent of the social, economic and health benefits of rehabilitation to be realized, timely, high quality and affordable rehabilitation interventions should be available to all. In many cases, this means starting rehabilitation as soon as a health condition is noted and continuing to deliver rehabilitation alongside other health interventions.
Unmet Global Need for Rehabilitation
Globally, about 2.4 billion people are currently living with a health condition that may benefit from rehabilitation. With changes taking place in the health and characteristics of the population worldwide, this estimated need for rehabilitation is only going to increase in the coming years. People are living longer, with the number of people over 60 years of age predicted to double by 2050, and more people are living with chronic diseases such as diabetes, stroke and cancer. At the same time, the ongoing incidence of injury and child developmental conditions (such as cerebral palsy) persist. These health conditions can impact an individual’s functioning and are linked to increased levels of disability, for which rehabilitation can be beneficial.
In many parts of the world, this increasing need for rehabilitation is going largely unmet. More than half of people living in some low- and middle-income countries who require rehabilitation services do not receive them.
Global rehabilitation needs continue to be unmet due to multiple factors, including:
- lack of prioritization, funding, policies, and plans for rehabilitation at a national level;
- lack of available rehabilitation services outside urban areas, and long waiting times;
- high out-of-pocket expenses and non-existent or inadequate means of funding;
- lack of trained rehabilitation professionals, with less than 10 skilled practitioners per 1 million population in many low- and middle-income settings;
- lack of resources, including assistive technology, equipment, and consumables;
- the need for more research and data on rehabilitation; and
- ineffective and under-utilized referral pathways to rehabilitation.
Rehabilitation in Emergencies
Natural hazards such as earthquakes or disease outbreaks and human induced hazards including conflict, terrorism or industrial accidents can generate overwhelming rehabilitation needs as a result of injury or illness. They also simultaneously disrupt existing services and have the greatest impact on the most vulnerable populations and the weakest health systems.
While the important role of rehabilitation in emergencies is recognized in clinical and humanitarian guidelines, it is rarely considered as part of health system preparedness and early response. The result is that pre-existing limitations in rehabilitation services are magnified, health service delivery is less efficient, and people directly affected are at risk of increased impairment and disability.
*The information was taken from https://www.who.int/news-room/fact-sheets/detail/rehabilitation
Classification of Rehabilitation
Medical rehabilitation — a branch of medicine that deals with the development or recovery of a person's physical, psychological, social, professional and educational potential according to his physiological or anatomical limitations, or - in case of stable health disorders - with the adaptation of the patient's life to the environment and society.
*The information was takes from https://likumi.lv/ta/id/44108-arstniecibas-likums
Professional rehabilitation — a set of measures that, after an individualized evaluation of functional impairments and determination of professional suitability, provides persons of working age with the acquisition or renewal of new professions, professional knowledge or skills, including the acquisition of vocational education programs at the basic and secondary education levels and multidisciplinary services for integration into the labor market.
Psychosocial rehabilitation — a direction of social rehabilitation that concerns a person and his family and whose purpose is to provide support in solving psychosocial problems.
Social functioning — a person's ability to function in various areas of life and fulfill appropriate social roles, which are constantly exposed to the influence of the surrounding environment and include society's expectations and objective requirements.
Social rehabilitation service — a set of measures aimed at restoring or improving social functioning abilities to ensure recovery of social status and integration into society, and includes services at the person's place of residence and social care and social rehabilitation institution or at the place of residence or social care and social rehabilitation institution.
*The information was taken from https://likumi.lv/ta/id/68488-socialo-pakalpojumu-un-socialas-palidzibas-likums
Physical Medicine
What Are Physical Agents?
Physical agents consist of energy and materials applied to patients to assist in their rehabilitation. Physical agents include heat, cold, water, pressure, sound, electromagnetic radiation, and electrical currents. The term physical agent can be used to describe the general type of energy, such as electromagnetic radiation or sound; a specific range within the general type, such as ultraviolet (UV) radiation or ultrasound; and the actual means of applying the energy, such as a UV lamp or an ultrasound transducer. The terms physical modality, biophysical agent, physical agent modality, electrophysical agent, and modality are alternatives for the term physical agent and are used interchangeably.
Clinical Pearl
Pearl Physical agents are energy and materials applied to patients to assist in their rehabilitation. Physical agents include heat, cold, water, pressure, sound, electromag-netic radiation, and electrical currents.
Categories of Physical Agents
| Category | Types | Clinical Examples |
| Thermal |
Superficial heating agents Deep-heating agents Cooling agents |
Hot pack, paraffin Ultrasound, diathermy Ice pack |
| Electromagnetic |
Electrical currents Electromagnetic fields |
TENS (TENS, Transcutaneous electrical nerve stimulation) Ultraviolet, laser |
| Mechanical |
Sound Water Traction Compression |
Ultrasound, shock waves Whirlpool Mechanical traction Elastic bandage, stockings |
Physical Therapy
Superficial Cold and Heat
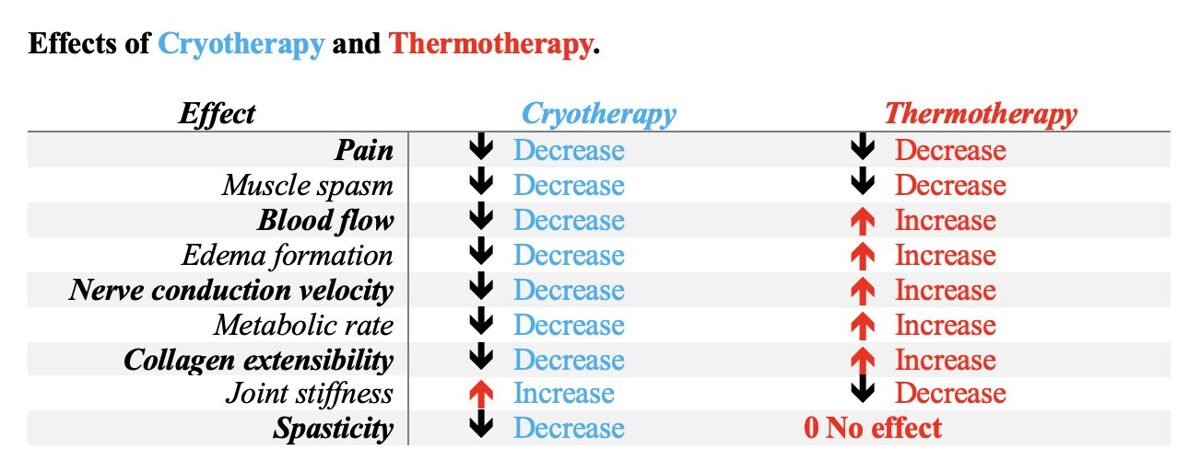
| Cryotherapy | Thermotherapy |
| I.Effects of Cold Þ Hemodynamic Effects Þ Neuromuscular Effects Þ Metabolic Effects | I. Effects of Heat Þ Hemodynamic Effects Þ Neuromuscular Effects Þ Metabolic Effects Þ Altered Tissue Extensibility |
| II.Clinical Indications for Cryotherapy ü Inflammation Control ü Edema Control ü Pain Control ü Modification of Spasticity ü Symptom Management in Multiple Sclerosis ü Facilitation | II.Clinical Indications for Superficial Heat ü Pain Control ü Increased Range of Motion and Decreased Joint Stiffness ü Accelerated Healing ü Infrared Radiation for Psoriasis |
| III.Contraindications and Precautions for Cryotherapy ý Contraindications for the Use of Cryotherapy ý Precautions for the Use of Cryotherapy | III.Contraindications and Precautions for Thermotherapy ý Contraindications for the Use of Thermotherapy ý Precautions for the Use of Thermotherapy |
| IV.Adverse Effects of Cryotherapy | IV.Adverse Effects of Thermotherapy Þ Burns Þ Fainting Þ Bleeding Þ Skin and Eye Damage From Infrared Radiation |
| V.Application Techniques T General Cryotherapy T Cold Packs or Ice Packs T Ice Massage T Controlled Cold Compression Unit T Vapocoolant Sprays and Brief Icing | V.Application Techniques ℃ General Superficial Thermotherapy ℃ Hot Packs ℃ Paraffin ℃ Fluidotherapy ℃ Infrared Lamps ℃ Contrast Bath |
· Fluidized therapy (Fluidotherapy) is a high-intensity heat modality consisting of a dry whirlpool of finely divided solid particles suspended in a heated air stream, the mixture having the properties of a liquid.
Choosing Between Cryotherapy and Thermotherapy